
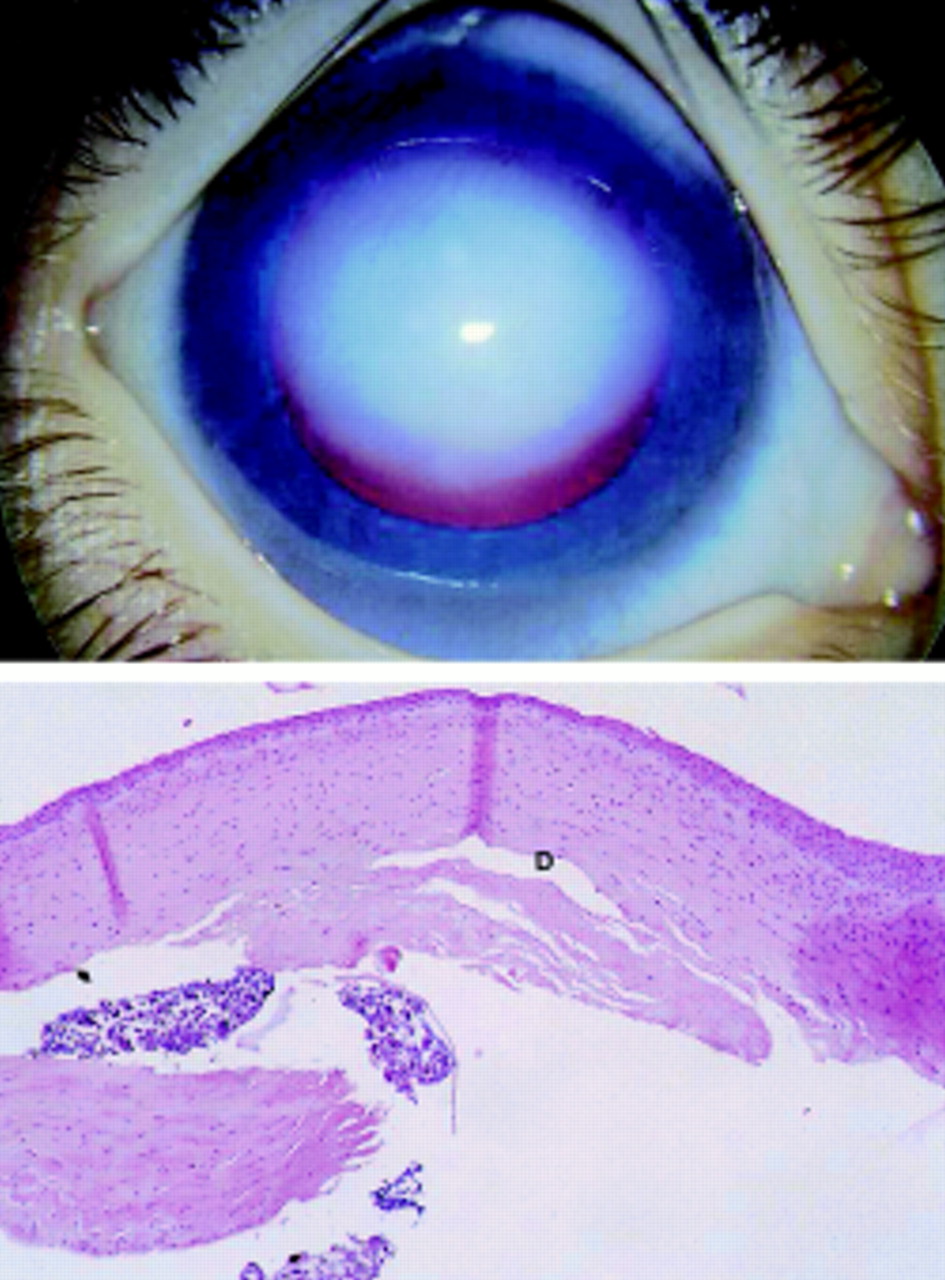
The diagnosis of Peters anomaly is made clinically with the finding of corneal opacification with corneal edema and underlying loss of Descemet's membrane and endothelium. Elevated intraocular pressure (IOP) typically presents in infancy, but can also arise later in life. Glaucoma is more common in those with cataracts or corneolenticular adhesions. Approximately 50-70% of patients with Peters anomaly have associated glaucoma. Patients with Peters anomaly are at increased risk of glaucoma, presumably due to abnormal development of the trabecular meshwork and Schlemm's canal and/or the presence of a shallow anterior chamber. 3: Small bilateral corneal opacities with associated iridocorneal adhesions in a patient with Peters anomaly. Peters anomaly has a wide spectrum of severity and corneal opacification is bilateral in approximately 80% of cases. Since then, Peters anomaly has been subdivided into three types: 1) Peters type I characterized by central corneal opacity with iridocorneal adhesions (Figure 3), 2) Peters anomaly type II with central corneal opacity and cataracts or corneolenticular adhesions, and 3) Peters-plus syndrome with Peters anomaly and short stature, developmental delay, dysmorphic facial features including cleft lip/palate along with cardiac and genital abnormalities. Peters anomaly was first described in 1906 by Albert Peters as a central corneal leukoma with variable synechiae between the iris and cornea and a defect in Descemet's membrane and the corneal endothelium. Peters anomaly is a rare eye malformation resulting in congenital corneal opacity and is part of a spectrum of developmental anomalies of the cornea, iris and lens termed "anterior segment dysgenesis." Discussion Clinical Features and Diagnosis Genetic testing was also done for two autosomal-dominant genes for Peters anomaly, PITX2 and FOXC1 genes, but the results were negative. At his 4-month postoperative visit, the graft was clear and there was visual improvement OD.

The patient subsequently underwent synechiolysis of iridocorneal adhesions and PKP in the right eye. However, to prevent amblyopia and provide visual rehabilitation a penetrating keratoplasty (PKP) of the right eye was recommended. The decision was made to observe the left eye as the corneal opacification had improved at his 1 month visit and there was an excellent view to the posterior pole. There was no evidence of glaucoma in either eye.

OS: Round 5 mm corneal opacity decentered nasally, but involving central visual axis inferononasal iridocorneal adhesion.OD: Diffuse corneal opacification with iridocorneal adhesion temporally minimal view of the anterior segment due to corneal opacity.Note the more significant corneal opacification in the right eye compared to the left. 2: Bilateral corneal opacities during examination under anesthesia.


 0 kommentar(er)
0 kommentar(er)
